Abstract
INTRODUCTION Pulmonary Embolism (PE) is the third most common cardiovascular condition. The American Society of Hematology recommends the use of direct oral anticoagulants (DOACs) over parenteral anticoagulant therapy with low molecular weight heparin (LMWH (parenteral AC)) with or without a Vitamin K antagonist (VKA) for initial PE treatment. There is limited data within our Canadian health region on how these therapeutic options are being used, and the trends of use over time.
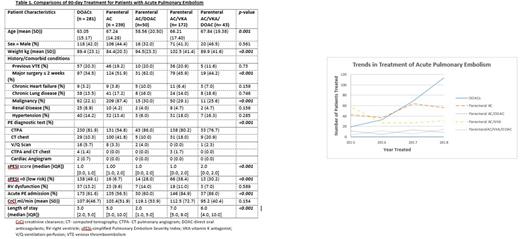
METHODS We completed a retrospective cohort study of outpatients with acute PE from June 1, 2014 to May 31, 2019 in one Canadian health region servicing a population of over 300,000. We identified patients with acute PE utilizing a search strategy of the Picture Archiving and Communication System (PACS) diagnostic imaging database for positive PE, including computed tomography (CT) reports, as well as a review of ventilation-perfusion (V/Q) scanning. Imaging reports were then manually reviewed to determine the presence of acute PE. Patients were included if they were aged ≥18 years, and the PE was diagnosed as an outpatient. Patients were excluded if the PE was diagnosed during hospital admission for another condition. Data collected by chart review up to 90 days after the diagnosis of PE included drug and patient-specific characteristics, and components of the simplified Pulmonary Embolism Severity Index (sPESI). Medication treatment of patients with PE were categorized into DOACs alone, parenteral AC alone, parenteral AC transitioned to VKA, parenteral AC transitioned to DOACs, and transition between the three ACs (parenteral, VKA, DOACs). DOACs alone included initial treatment with therapeutic LMWH up to 10 days, and parenteral AC transitioned to DOACs comprised treatment with parenteral AC>10 days prior to switching to a DOAC. Data are reported as means and standard deviations for continuous variables or percentages for categorical variables. Patient characteristics and treatments are compared using chi-square and analysis of variance tests. Multinomial logistic regression was used to determine the predictors of acute PE treatment.
RESULTS A total of 785 patients with PE were diagnosed as an outpatient, with mean age of 63.4 ± 15.9 years, 42.3% male, and mean weight of 92.0 ± 30.4 kg. There were 247 (31.5%) patients with a sPESI score = 0, and 521 (66.4%) were admitted to hospital for treatment of the acute PE. Treatments utilized included DOACs alone (n=281, 35.8%), parenteral anticoagulants alone (n=239, 30.4%) or combined with VKA (n=172, 21.9%), parenteral anticoagulants followed by DOACs (n=50, 6.4%) or parenteral anticoagulant combined with VKA switched to DOACs (n=43, 5.5%) (Table 1). Significant differences in patient characteristics between treatment groups included: mean age (p=0.001), mean weight (p<0.001), history of malignancy (p< 0.001), mean sPESI score (p<0.001) and low risk PE (sPESI=0) (p=<0.001), admission to hospital for PE treatment (p< 0.001) and length of stay for acute PE (p<0.001). Multinomial logistic regression showed that compared to parenteral anticoagulants alone, patients with a history of malignancy were less likely to be treated with DOACs (RR 0.06, 95% CI 0.03-0.11), parenteral anticoagulants transitioned to DOACs (RR 0.07, 95% CI 0.03-0.018), parenteral anticoagulants transitioned to VKA (RR 0.11, 95% CI 0.06 -0.20), or parenteral anticoagulants transitioned to VKA then DOACs (RR 0.05, 95% CI 0.02-0.13). Compared to parenteral anticoagulants alone, patients admitted to hospital for acute PE treatment were more likely to receive parenteral anticoagulants transitioned to VKA (RR 2.94, 95% CI 1.64 - 5.23), or parenteral anticoagulants transitioned to VKA then DOACs (RR 3.76, 95% CI 1.21 -11.65). Trends in anticoagulant use over the the period of study showed an increasing use of DOACs as initial treatment (Figure 1).
CONCLUSION In our study, over a five year period, patients with acute PE and malignancy were more likely to be prescribed parenteral anticoagulation alone compared to other treatment options. Patients with acute PE admitted to hospital were more likely to be prescribed parenteral anticoagulants transitioned to VKA, or parenteral anticoagulants transitioned to VKA then switched to DOACs. The use of DOACs trended upwards for treatment of acute PE over the time period examined. Further analysis is ongoing to determine additional clinical and economic outcomes.
Disclosures
Young:Bayer Canada: Research Funding; Pfizer: Honoraria; Sanofi Canada: Research Funding. Bonsu:Sanofi Canada: Research Funding. Lee:Shoppers Drug Mart: Research Funding. Chitsike:Pfizer: Honoraria; Bayer Canada: Research Funding; Sanofi Canada: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.